HR COBRA Continuation of Coverage Request Template Word
The HR COBRA Continuation of Coverage Request Template Word is a comprehensive and easy-to-use tool designed to help businesses comply with the Consolidated Omnibus Budget Reconciliation Act (COBRA) regulations. This template is specifically designed to help HR professionals manage the process of providing continuation of coverage to employees who have lost their job or experienced a reduction in work hours.
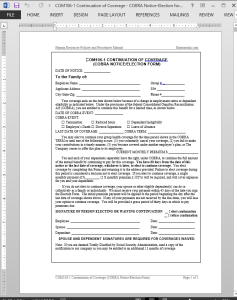
The HR COBRA Continuation of Coverage Request Template Word is a customizable document that can be easily tailored to meet the specific needs of your organization. It includes all the necessary information and forms required by law, including the COBRA election notice, the COBRA continuation coverage request form, and the COBRA premium payment notice.
With this template, you can streamline the COBRA process and ensure that your organization is in compliance with all the relevant regulations. It provides a clear and concise framework for managing the COBRA process, from initial notification to final termination of coverage.
The HR COBRA Continuation of Coverage Request Template Word is an essential tool for any HR professional who wants to ensure that their organization is in compliance with COBRA regulations. It is easy to use, customizable, and provides all the necessary forms and information required by law. With this template, you can simplify the COBRA process and ensure that your organization is protected from potential legal liabilities.
COBRA Continuation of Coverage Request Template
Plan administrators, upon receiving notice of a qualifying event, must provide an election notice – COBRA Continuation of Coverage Request Template – to the qualified beneficiaries of their right to elect COBRA coverage. COM106-1 CONTINUATION OF COVERAGE (COBRA NOTICE/ELECTION FORM) must be provided in person or by first class mail within 14 days after the plan administrator receives notice that a qualifying event has occurred.
There are two special exceptions to the notice requirements for multi-employer plans. First, the period for providing notices may be extended beyond the 14- and 30-day requirements if allowed by plan rules. Second, if the plan rules allow, employers may be relieved of the obligation to notify plan administrators when employees terminate or reduce their work hours. Plan administrators would then be responsible for determining whether these qualifying events have occurred.
COBRA continuation coverage can be terminated for the following reasons:
- On the date that the employer ends a group health plan to all employees.
- At the time that the qualifying beneficiary becomes qualified to participate in another group plan offered from new employment.
- If the beneficiary fails to make timely payments to the provider for the continuation coverage.
- The date on which a qualified beneficiary is entitled to benefits under Medicare.
 COBRA Continuation of Coverage Request Template Details
COBRA Continuation of Coverage Request Template Details
Pages: 01
Words: 449
Format: Microsoft Word 2013 (.docx)
Language: English
Manual: Human Resources
Category: Compensation
Procedure: Consolidated Budget Reconciliation Procedure COBRA COM106
Type: Form




Reviews
There are no reviews yet.